New Covid-19 Strain: What do we know?
January 23, 2021
“We’re far from being out of the woods,” claimed Michael Johansson, Ph.D., a member of the CDC’s COVID-19 Response Team.
The Coronavirus, a severe acute respiratory syndrome (SARS-CoV-2), was first identified as the source of a pneumonia outbreak in Wuhan, China. Months later, this virus would spread across the world and become the pandemic to haunt the 21st Century. However, in September 2020, a mutation of the Coronavirus was detected in South East England. Within months, this “new virus” has become responsible for a whopping 60 percent of all cases in London and its surrounding areas. While many nations were just beginning to recover from the original surge, another outbreak was beginning to emerge.
The B.1.1.7 “super strain” has emerged alongside recent variants found in South Africa and Brazil called 1.341 and P.1. The B.1.1.7 strain is predicted to account for the majority of U.S. COVID cases by March 2021. According to CDC Modeling, “Increased SARS-CoV-2 transmission might threaten strained health care resources, require extended and more rigorous implementation of public health strategies, and increase the percentage of population immunity required for pandemic control.”
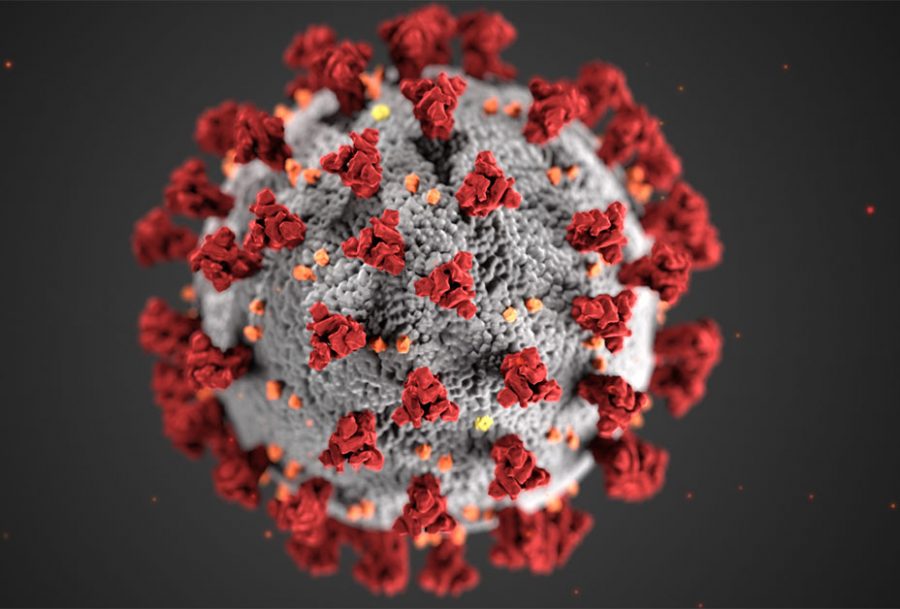
Early research has shown this new strain to have around 23 genetic changes, making it more deadly for the human population. Specifically, mutations have occurred on the spikes of proteins (antigens); if mutated enough, the immune systems’ white blood cells – which are specific defense mechanisms against pathogens – will not effectively protect the internal tissue and organs of the body. Many scientists have been researching the possible effects of the released vaccines on this new mutation and question as to whether the generated antibodies will hold up against the B.1.1.7 strain.
According to the CDC, there is currently “no known difference in clinical outcomes associated with the described SARS-CoV-2 variants.” However, due to higher rates of transmission, the variants lead to more cases, “exacerbating the burden on an already strained health care system, and resulting in more deaths.”
As of now, the CDC has not yet released new prevention measures to limit the spread of the B.1.1.7 strain. However, it can be assumed that complying with the currently released public health measures will help reduce the potential impact of the mutated virus. These precautions, including physical distancing, mask-wearing, handwashing, hygiene, quarantining, and vaccination, have been proven effective and are the best means of slowing the spread of the virus, regardless of the strain. Doing so will give time for in-depth research of the specific mutation, variants, and needed vaccination alterations which will, ultimately, decrease the severity and spread in the human population.
Looking at the recent vaccine rollout, including the Moderna and Pfizer vaccines, there has been skepticism surrounding their effectiveness towards the mutation. BioNTech, a partner with Pfizer, has recently stated their confidence that “the vaccine will be able to deal with the mutations.” Additionally, since the current vaccines have been developed with mRNA technology, changing the vaccine will be relatively quick, taking generally only six weeks in time.
In the future, the CDC has stressed the importance of continuing precautions. Modeling has shown the possibility of the mutation to make up around 50% percent of the cases by this March. Due to the contagious nature of the variants, the importance of limiting the spread is more important than ever. Michael Johansson, a member of the CDC’s COVID response team, stated they recognize “that people are tired, and for some it’s getting harder and harder to social distance and wear their masks, but we have to do what we can now.” COVID fatigue is becoming more prevalent; however, the importance of taking safety measures seriously is more important than ever.